Stages of Congestive Heart Failure: Know the Warning Signs!

Cardiovascular diseases claim nearly 18 million lives globally each year, with congestive heart failure affecting millions of Indians across all demographics. Understanding the progression of this condition is vital for both patients and their caregivers. When armed with knowledge about the stages of congestive heart failure, you gain power over your health journey and can make informed decisions alongside your healthcare team. This comprehensive guide walks you through each stage of congestive heart failure, from risk factors to advanced management, with a focus on practical information relevant to Indian patients and families.
What is Congestive Heart Failure?
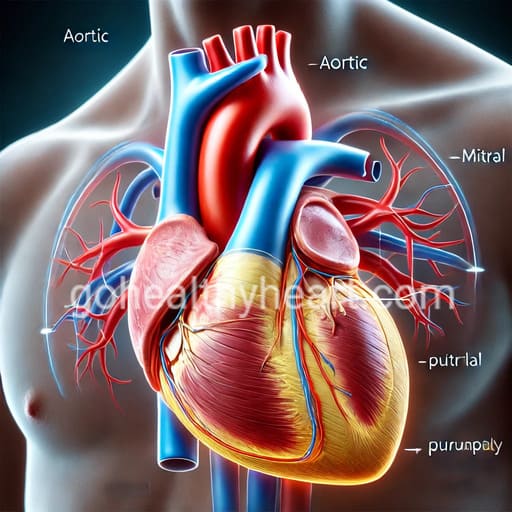
Congestive heart failure occurs when your heart cannot pump blood efficiently enough to meet your body’s needs. Unlike a sudden heart attack, heart failure typically develops gradually as the heart muscle weakens or stiffens over time. This inefficient pumping leads to congestion – a buildup of fluid in various parts of the body, particularly the lungs, ankles, and abdomen.
Your heart is a remarkable organ, normally pumping about 5 liters of blood every minute. In heart failure, this pumping capacity diminishes, causing blood to back up and fluid to leak into surrounding tissues. The condition can affect the left side of the heart (responsible for pumping blood to the body), the right side (which sends blood to the lungs), or both sides simultaneously.
Common causes of heart failure in India include coronary artery disease, long-term hypertension, and diabetes – conditions increasingly prevalent in our population. Other causes include heart valve problems, congenital heart defects, certain infections, and cardiomyopathy (disease of the heart muscle). Recognizing these causes is crucial for prevention and early intervention.
Understanding the Classification Systems for Heart Failure
Medical professionals use two primary systems to classify heart failure. The first is the American College of Cardiology/American Heart Association (ACC/AHA) staging system, which categorizes heart failure into Stages A through D based on disease progression and structural changes to the heart. This system is particularly useful for treatment planning as it addresses the full spectrum from risk factors to advanced disease.
The second classification is the New York Heart Association (NYHA) Functional Classification, which divides heart failure into Classes I through IV based on how symptoms affect daily activities. A patient may be categorized in both systems simultaneously – for example, someone might have Stage C heart failure (structural disease with symptoms) while experiencing Class II limitations (slight limitation of physical activity).
These classifications help your doctor communicate about your condition precisely and determine the most appropriate treatments for your specific situation. Understanding which stage or class applies to you can help you better comprehend your doctor’s recommendations and what to expect in the future.
Stage A: At Risk for Heart Failure
Stage A represents individuals who don’t have heart damage or symptoms yet but face high risk for developing heart failure. If you have hypertension, diabetes, metabolic syndrome, coronary artery disease, or a family history of cardiomyopathy, you fall into this category. In India, where these conditions are increasingly common due to changing lifestyles, Stage A represents a critical opportunity for prevention.
Prevention at this stage focuses primarily on aggressive management of risk factors. Controlling blood pressure, managing diabetes, maintaining healthy cholesterol levels, and avoiding tobacco are essential strategies. Regular physical activity of at least 150 minutes per week, following a heart-healthy diet low in salt and saturated fats, and maintaining a healthy weight can significantly reduce your risk of progression.
Medications may be prescribed to manage underlying conditions like hypertension or diabetes. Regular check-ups with your doctor are important for monitoring your heart health and adjusting prevention strategies as needed.
The good news about Stage A is that with proper lifestyle modifications and medical management, many people can prevent heart failure from ever developing. Taking action at this early stage offers the greatest opportunity to maintain heart health throughout your life.
Stage B: Structural Heart Disease Without Symptoms
Stage B marks a significant transition – your heart now shows structural abnormalities, but you still feel normal in your daily activities. You might have an enlarged heart (cardiomegaly), evidence of a previous heart attack, valve disease, or low ejection fraction (a measure of how effectively your heart pumps blood), yet experience no shortness of breath, fatigue, or swelling.
This “silent” stage is typically discovered during routine check-ups or tests done for other reasons. An echocardiogram, electrocardiogram (ECG), or other cardiac imaging might reveal these structural changes before symptoms appear. This underscores the importance of regular medical check-ups, especially if you have risk factors for heart disease.
Treatment at Stage B aims to prevent further heart damage and delay symptom onset. Your doctor may prescribe medications such as ACE inhibitors, angiotensin receptor blockers (ARBs), or beta-blockers, which have been shown to protect the heart. In some cases, surgical interventions to correct valve problems or implantable devices might be recommended to prevent progression.
The lifestyle changes recommended for Stage A become even more crucial at Stage B. Regular exercise (with your doctor’s guidance), heart-healthy eating habits, strict management of other health conditions, and avoiding alcohol and tobacco can help preserve your remaining heart function and prevent symptom development.
Stage C: Structural Heart Disease With Previous or Current Symptoms
Stage C represents a significant progression – you now have structural heart disease and either currently experience symptoms or have experienced them in the past. Common symptoms include shortness of breath (especially when lying down or during exertion), fatigue, reduced exercise capacity, and swelling in the ankles, feet, legs, or abdomen. These symptoms occur because your heart cannot pump efficiently enough to meet your body’s demands or cannot properly handle the blood returning from your body.
Daily activities may become challenging as symptoms can fluctuate – you might feel relatively well one day and overwhelmed by fatigue the next. This inconsistency can be frustrating and affect your quality of life. Tracking your symptoms, weight, and fluid intake can help you and your doctor identify patterns and adjust treatment accordingly.
Medical management becomes more intensive at this stage. In addition to the medications used in Stage B, diuretics are often prescribed to reduce fluid buildup. Aldosterone antagonists, hydralazine with nitrates, or newer medications like SGLT2 inhibitors might be added to your regimen. Your doctor will carefully monitor kidney function, electrolytes, and blood pressure as these medications can affect these parameters.
Self-care becomes vitally important at Stage C. Learning to monitor your condition through daily weight checks, recognizing warning signs of worsening heart failure, and understanding when to contact your healthcare provider can prevent hospitalizations. Many patients benefit from cardiac rehabilitation programs that provide supervised exercise and education. Support groups, either in-person or online, can also provide valuable emotional support and practical advice from others navigating similar challenges.
Stage D: Advanced Heart Failure
Stage D represents advanced or refractory heart failure – symptoms occur at rest despite maximal medical therapy. Daily activities become severely limited, and hospital admissions are frequent. Quality of life is significantly impacted, and specialized interventions beyond standard treatments are usually considered.
Advanced treatments available in India include mechanical circulatory support devices like left ventricular assist devices (LVADs), which can help your heart pump more effectively. Heart transplantation may be an option for suitable candidates at specialized centers in metropolitan areas. Continuous inotropic therapy (medications that strengthen heart contractions) may be used for symptom management in some cases.
At this stage, discussions about your care preferences become increasingly important. Palliative care, which focuses on symptom management and quality of life rather than cure, can be integrated with other treatments. This approach doesn’t mean giving up – rather, it ensures your comfort and dignity while medical treatments continue as appropriate.
Family support becomes even more crucial at Stage D. Caregivers may need to assist with medication management, transportation to frequent medical appointments, and daily activities. Connecting with social services and community resources can provide valuable support for both patients and family members navigating this challenging stage.
Treatment Approaches Across All Stages
A comprehensive approach to heart failure management spans all stages of the condition. Medications form the foundation of treatment, with different combinations used according to stage, symptoms, and individual factors. Regular monitoring allows your doctor to adjust medications for optimal benefit while minimizing side effects.
Devices such as implantable cardioverter-defibrillators (ICDs) or cardiac resynchronization therapy (CRT) may benefit selected patients with specific types of heart failure. Surgical interventions to address underlying causes – such as coronary artery bypass grafting for blocked arteries or valve repair/replacement – might be recommended in appropriate cases.
Lifestyle modifications remain important throughout all stages. A diet low in sodium (less than 2g daily) helps prevent fluid retention. For Indian patients, this means being mindful of salt in home cooking and prepared foods – many traditional Indian dishes can be adapted to be heart-healthy without sacrificing flavor by using herbs and spices instead of salt.
Regular physical activity, tailored to your capabilities and guided by healthcare providers, strengthens your body and can improve heart function. Even at advanced stages, appropriate exercise can help maintain independence and quality of life. In India, yoga and pranayama (breathing exercises) can complement conventional exercise recommendations, offering both physical and stress-reduction benefits when practiced appropriately.
Living Well with Heart Failure
Despite the challenges of heart failure, many patients lead fulfilling lives with proper management. Creating a sustainable daily routine that balances activity with rest helps conserve energy for what matters most to you. Breaking tasks into smaller segments and prioritizing important activities can help you accomplish more without excessive fatigue.
Dietary adaptations are essential but need not be overly restrictive. Working with a dietitian familiar with Indian cuisine can help you modify favorite dishes to be heart-healthy. For example, using less oil in cooking, reducing salt, incorporating more vegetables and whole grains, and limiting processed foods can make significant differences in your heart health.
Emotional well-being deserves attention alongside physical health. Heart failure can trigger anxiety, depression, and fear about the future – all normal responses to a chronic condition. Connecting with others through support groups, seeking counseling when needed, and practicing stress-reduction techniques like meditation can improve your psychological resilience and overall quality of life.
Maintaining open communication with your healthcare team ensures you receive appropriate care as your condition changes. Prepare for appointments by noting any symptom changes, medication concerns, or questions that have arisen since your last visit. Bringing a family member to appointments can help ensure important information is understood and remembered.
When to Seek Emergency Care
Knowing when to seek urgent medical attention is vital for heart failure patients. Call your doctor immediately or go to the emergency room if you experience sudden weight gain (2-3 kg within 1-2 days), increased swelling, progressive shortness of breath, difficulty breathing while lying flat, chest pain, palpitations, dizziness, or confusion. These symptoms may indicate worsening heart failure requiring prompt intervention.
Keep an updated list of your medications, allergies, and doctor contact information readily available for emergencies. India’s growing network of emergency cardiac care centers means timely intervention is increasingly accessible, particularly in urban areas. Familiarize yourself with the nearest cardiac emergency facilities to your home and workplace.
Creating an emergency plan with family members ensures everyone knows what to do in a crisis. This includes who to call, which hospital to go to, and what information to provide to emergency responders. Being prepared reduces stress and enables faster appropriate care when minutes matter.
Frequently Asked Questions
A heart attack (myocardial infarction) occurs suddenly when blood flow to a section of heart muscle becomes blocked, causing tissue damage or death. Heart failure, by contrast, is a chronic condition where the heart cannot pump efficiently enough to meet the body’s needs. While a heart attack can lead to heart failure, many other conditions can cause heart failure as well. Heart attacks typically cause sudden, intense symptoms, while heart failure symptoms often develop gradually over time.
In some cases, heart failure can be reversed, particularly if it’s caused by a treatable condition like valve disease, anemia, or thyroid problems. Early stages of heart failure may show significant improvement with proper treatment and lifestyle changes. However, in many cases, the goal of treatment is to manage the condition and prevent progression rather than achieve complete reversal. Even without full reversal, proper treatment can significantly improve symptoms and quality of life.
Life expectancy varies greatly depending on many factors, including the stage of heart failure, underlying causes, age, other health conditions, and response to treatment. With modern treatments, many patients live for years or even decades after diagnosis, particularly those diagnosed at earlier stages. Rather than focusing on statistics, work with your doctor to optimize your individual treatment plan and focus on quality of life and symptom management.
Ejection fraction (EF) is a measurement of how much blood your heart pumps out with each contraction, expressed as a percentage. A normal EF is typically between 55-70%. In heart failure with reduced ejection fraction (HFrEF), the EF falls below 40%. In heart failure with preserved ejection fraction (HFpEF), the EF remains normal, but the heart doesn’t fill properly. EF helps determine the type of heart failure and guides treatment decisions, but it’s just one of many factors considered when staging heart failure.
A heart-healthy diet for congestive heart failure typically includes limiting sodium to 2,000 mg or less per day, restricting fluid intake if recommended by your doctor, eating plenty of fruits and vegetables, choosing whole grains, and limiting saturated fats and added sugars. For Indian patients, this might mean adapting traditional recipes by using less salt and oil, incorporating more plant-based proteins, and being mindful of hidden sodium in packaged foods and pickles. Working with a dietitian familiar with Indian cuisine can help you create a sustainable eating plan that supports heart health while respecting cultural food preferences.
While some Ayurvedic and natural approaches may offer supportive benefits for overall cardiovascular health, they should never replace conventional medical treatment for heart failure. Some herbs and supplements may interact with heart failure medications or affect heart function. Always discuss any complementary approaches with your cardiologist before trying them. Certain aspects of Ayurveda, such as stress management techniques and appropriate physical activity like yoga (when medically approved), can complement conventional care as part of a holistic approach to wellness.
The frequency of medical visits depends on your heart failure stage, stability, and individual needs. Newly diagnosed patients or those with recent medication changes might need appointments every 2-4 weeks. Stable patients might see their cardiologist every 3-6 months. Regular monitoring of weight, blood pressure, and symptoms between visits helps your healthcare team adjust treatment as needed. Telehealth options are increasingly available in India, allowing for more frequent check-ins without the need for in-person visits in some cases.
Yes, appropriate exercise is actually beneficial for most heart failure patients. Your doctor can help determine what types and amounts of exercise are safe for you based on your heart failure stage and overall health. Generally, low to moderate intensity activities like walking, swimming, or cycling are recommended, starting with short durations and gradually increasing as tolerated. Many patients benefit from structured cardiac rehabilitation programs where exercise is supervised by healthcare professionals. Always stop exercising and contact your doctor if you experience increased shortness of breath, chest pain, dizziness, or unusual fatigue.
Warning signs of worsening heart failure include increased shortness of breath (especially with minimal exertion or when lying down), sudden weight gain (2-3 kg in a few days), increased swelling in the legs or abdomen, persistent cough or wheezing, increased fatigue or weakness, loss of appetite, confusion or impaired thinking, and increased heart rate or palpitations. Keeping a daily log of weight, symptoms, and activity levels can help you recognize concerning patterns early. Contact your healthcare provider promptly if you notice these warning signs rather than waiting for your next scheduled appointment.
Family support is crucial for heart failure patients. Practical assistance might include helping with medication management, accompanying the patient to medical appointments, and assisting with heart-healthy meal preparation. Emotional support through listening, encouraging adherence to treatment plans without nagging, and acknowledging the challenges of living with heart failure is equally important. Family members should also learn to recognize warning signs of worsening heart failure and know when to seek emergency care. Taking care of their own health and well-being is essential too, as caregiver burnout can affect the quality of support they provide.
Conclusion
Understanding the stages of congestive heart failure empowers you to take an active role in your heart health journey. From prevention in the early stages to specialized care in advanced disease, knowledge guides decision-making and improves outcomes. With appropriate medical care, lifestyle modifications, and support systems, many heart failure patients maintain good quality of life despite their condition.
Heart failure management is a partnership between you, your family, and your healthcare team. By working together, monitoring your condition carefully, and making heart-healthy choices daily, you can effectively manage heart failure at any stage. New treatments continue to emerge, offering hope and improved options for patients at all stages of heart failure.
For regular updates on cardiac health and the latest in heart failure management, visit gohealthyheart.com. Remember that while heart failure is a serious condition, it doesn’t define you – with proper care and support, you can continue to live a meaningful life focused on what matters most to you.



One thought on “Stages of Congestive Heart Failure: Know the Warning Signs!”
Comments are closed.