Heart Valve Problems: Warning Signs You Shouldn’t Ignore
By Dr. Nageswara Rao Goteti, Interventional Cardiologist, Vijayawada
Introduction
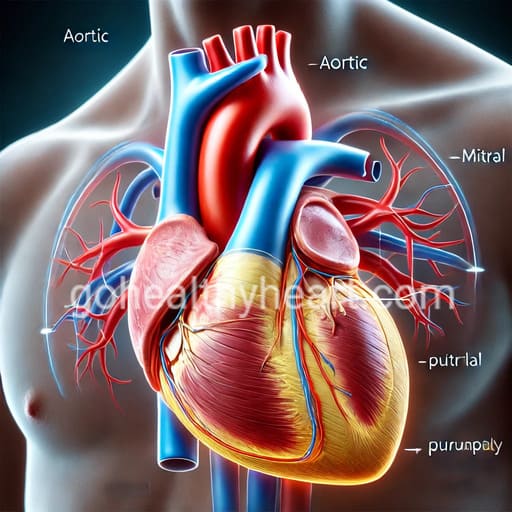
Your heart, a remarkable organ roughly the size of your fist, performs the crucial task of pumping oxygen-rich blood throughout your body. At its core are four vital valves—mitral, aortic, tricuspid, and pulmonary—each playing an indispensable role in maintaining proper blood flow.
When these valves malfunction, the signs of heart valve problems can develop gradually, often going unnoticed until significant damage has occurred. Understanding these warning signs is crucial for early detection and successful treatment.
Understanding Heart Valve Function and Disease
Your heart’s four valves function as sophisticated one-way gates, ensuring blood flows in the correct direction through your heart’s chambers. Each valve opens and closes approximately 100,000 times per day, coordinating perfectly to maintain proper blood flow and prevent backflow.
Heart valve disease can manifest in several ways, each presenting unique challenges. The most common form is valve stenosis, where the valve opening narrows, forcing your heart to work harder to pump blood through the constricted passage. This condition commonly affects the aortic valve, though any valve can be impacted.
Another type is valve regurgitation, also known as valve insufficiency or a leaky valve. This occurs when a valve doesn’t close completely, allowing blood to flow backward and reducing the heart’s pumping efficiency. The mitral valve is particularly susceptible to this condition.
In rare cases, valve atresia may occur, where a valve lacks a proper opening for blood flow. Present from birth, this condition requires immediate medical attention and often necessitates surgical intervention.
Recognizing Early Warning Signs
The initial signs of heart valve problems can be subtle and easily overlooked. Many patients first notice changes in their exercise tolerance. You might find yourself experiencing unexpected difficulty completing routine physical activities or needing to stop and rest during familiar tasks. Even climbing stairs might leave you feeling more winded than usual.
Subtle energy changes often accompany early valve problems. You might experience increasing fatigue during daily activities or need more recovery time after physical exertion. An unexplained decrease in overall energy levels could be your body’s way of signaling that something isn’t quite right.
Progressive Symptoms
As valve disease advances, more noticeable symptoms typically emerge. Breathing difficulties become more pronounced. You might experience shortness of breath during mild activity or find it difficult to breathe when lying flat, a condition known as orthopnea. Some patients wake up breathless in the middle of the night, experiencing what doctors call paroxysmal nocturnal dyspnea.
Circulatory problems often become apparent as the condition progresses. You might notice swelling in your ankles, feet, and legs, particularly after standing or sitting for long periods. Some patients experience abdominal bloating or visible neck vein distention. Your extremities might feel colder than usual due to reduced circulation.
Cardiac symptoms can become more prominent. Heart palpitations or irregular heartbeat patterns might develop. You could experience chest pain or pressure, especially during physical activity. During medical examinations, your doctor might detect heart murmurs, which are unusual sounds caused by turbulent blood flow through the affected valve.
Risk Factors and Causes
Age plays a significant role in valve disease development. Natural valve degeneration occurs over time, and calcium can build up on valve tissue. The heart muscle and supporting structures may weaken with age, contributing to valve problems.
Several medical conditions can increase your risk of developing valve problems. A history of rheumatic fever can cause permanent valve damage. Endocarditis, an infection of the heart valve, can lead to serious complications. High blood pressure and atherosclerosis put additional stress on your heart valves.
Genetic and congenital factors also play a role. Some people are born with heart valve defects or have inherited conditions like Marfan syndrome that affect heart valve function. A family history of heart valve disease may increase your risk of developing similar problems.
Diagnosis and Assessment
Diagnosing heart valve problems begins with a thorough evaluation. Your healthcare provider will take a detailed medical history and perform a physical examination. They’ll listen carefully for heart murmurs and assess your symptoms and risk factors.
Various diagnostic tests help confirm the presence and severity of valve problems. Non-invasive tests like echocardiograms use ultrasound to visualize valve structure and function. Electrocardiograms (ECG/EKG) help assess heart rhythm and detect irregularities. Chest X-rays can show changes in heart size or shape.
Advanced imaging techniques provide even more detailed information. Cardiac MRI and CT scans offer precise views of valve structure and function. 3D echo imaging helps plan surgical interventions when necessary. Nuclear medicine studies can assess blood flow patterns through the heart.
Treatment Approaches
Treatment for heart valve problems varies depending on the severity and type of condition. For mild cases, conservative management might be appropriate. This includes regular monitoring, risk factor modification, and lifestyle adjustments to reduce strain on your heart.
Medical therapy often plays a crucial role. Your doctor might prescribe medications to manage symptoms and prevent complications. These could include anticoagulants to prevent blood clots, beta-blockers to control heart rate, or diuretics to reduce fluid buildup.
Surgical intervention becomes necessary in some cases. Valve repair procedures like valvuloplasty or annuloplasty can restore proper valve function. In more severe cases, valve replacement might be needed. Options include mechanical valves, biological valves, or newer transcatheter procedures for suitable candidates.
Living with Heart Valve Disease
Managing heart valve disease requires ongoing attention to your health. Regular medical check-ups help monitor your condition and adjust treatment as needed. Tracking your symptoms and maintaining medication compliance are essential aspects of successful management.
Quality of life remains a priority. Many patients benefit from cardiac rehabilitation programs that help them stay active safely. Emotional support, whether from family, friends, or support groups, plays a vital role in coping with the challenges of heart valve disease.
Frequently Asked Questions
Not all heart valve problems require immediate attention, but certain symptoms should never be ignored. Severe chest pain, fainting episodes, or sudden severe shortness of breath require emergency care. Even milder symptoms like increasing fatigue or mild breathlessness should be evaluated by a healthcare provider, as early intervention often leads to better outcomes.
While some heart valve problems, particularly those present from birth, cannot be prevented, you can reduce your risk of developing valve disease. Maintaining healthy blood pressure, promptly treating strep throat infections, and following a heart-healthy lifestyle can help prevent valve damage. Regular exercise, a balanced diet, and avoiding tobacco use are essential preventive measures.
While both conditions affect the heart, they are quite different. Heart valve problems involve structural issues with the heart’s valves that affect blood flow. A heart attack occurs when blood flow to a portion of the heart muscle is blocked. However, some symptoms may overlap, which is why any chest pain or discomfort should be evaluated by a medical professional.
The frequency of valve check-ups depends on your age, risk factors, and whether you have existing valve issues. Generally, adults over 65 should have regular heart examinations, including listening for murmurs. If you have known valve disease, your cardiologist will establish a personalized monitoring schedule.
Pregnancy puts additional stress on the heart, and women with existing valve conditions need careful monitoring during pregnancy. If you have a heart valve condition and are planning pregnancy, discuss this with your healthcare provider. Many women with valve conditions have successful pregnancies with proper medical supervision.
Conclusion
Understanding heart valve problems and recognizing their signs can make a significant difference in treatment outcomes. While some valve conditions develop slowly, others may require immediate medical attention. Regular check-ups and awareness of symptoms help ensure timely intervention and better outcomes.
If you experience any concerning symptoms, don’t hesitate to consult your healthcare provider. For more reliable information about heart health and cardiac conditions, visit gohealthyheart.com.
Remember, this information serves as a guide and should not replace professional medical advice. Always consult with your healthcare provider for personalized recommendations and treatment plans.




One thought on “Heart Valve Problems: Warning Signs You Shouldn’t Ignore”
Comments are closed.