Congenital Heart Defects in Newborns: Diagnosis and Treatment
Introduction:
Congenital heart defects in newborns (CHDs) are the most common birth defects, affecting about 1 in every 100 babies globally. That means roughly 1% of newborns come into the world with some form of heart abnormality, ranging from mild to life-threatening. For any new parent, the idea of their baby having a heart problem can be terrifying. But there’s good news—thanks to modern medical advances, most children with CHDs grow up to lead healthy, active lives.
In this article, we’ll walk you through everything you need to know about CHDs, from how they’re diagnosed right after birth (and sometimes even before!) to the different treatment options available. Whether you’re a parent, healthcare provider, or just someone wanting to understand this complex topic better, we’re here to break it down for you.
What Are Congenital Heart Defects (CHDs)?
Congenital heart defects are structural problems with the heart that are present at birth. These defects can affect how blood flows through the heart and to the rest of the body. Some defects are mild and cause few or no symptoms, while others can result in serious, life-threatening complications.
The most common types of CHDs fall into two broad categories:
- Cyanotic heart defects: These cause low oxygen levels in the blood, often leading to a bluish tint to the skin, lips, and fingernails.
- Acyanotic heart defects: These do not usually affect oxygen levels as severely but can still cause issues with the heart’s ability to pump blood properly.
The impact of a CHD on a newborn depends on the size, location, and complexity of the defect. Some defects resolve on their own over time, while others may require immediate medical or surgical intervention.
Signs and Symptoms of Congenital Heart Defects in Newborns
In the first few days or weeks of life, newborns with CHDs might display symptoms that indicate something is wrong with their heart. Early diagnosis is crucial because timely treatment can make a significant difference in the child’s prognosis. Here are some signs that could indicate a CHD:
- Bluish tint to the skin (cyanosis), particularly around the lips and fingernails.
- Rapid or labored breathing, even when the baby is at rest.
- Poor feeding or difficulty gaining weight, as the baby may struggle with energy levels.
- Sweating during feedings, a sign of the heart working too hard.
- Heart murmurs, which are often detected during a routine check-up but may require further investigation.
Symptoms can range from subtle to severe, depending on the type of defect. In some cases, the signs may not show up until later in infancy, especially with milder heart defects.
Methods for Diagnosing Congenital Heart Defects
Early detection of CHDs is critical for successful treatment. There are several ways doctors can diagnose congenital heart defects in newborns, starting from prenatal screenings to post-birth evaluations.
- Prenatal Screening: Many CHDs are detected before birth through a fetal echocardiogram, an ultrasound of the baby’s heart. This allows doctors to plan for immediate care after delivery if needed.
- Pulse Oximetry: This simple, non-invasive test measures how much oxygen is in the baby’s blood. A low oxygen level can be a sign of a heart defect and usually leads to further testing.
- Echocardiogram: After birth, an echocardiogram is the most definitive test for diagnosing a CHD. This ultrasound of the heart provides a detailed look at its structure and function, allowing pediatric cardiologists to pinpoint any abnormalities.
- Genetic Testing: Since some CHDs are linked to genetic disorders, doctors may also recommend genetic testing to see if a genetic syndrome is contributing to the defect.
Diagnosing a CHD early on gives the medical team the chance to develop a treatment plan and ensure the baby gets the best possible start.
Common Types of Congenital Heart Defects in Newborns
There are many types of congenital heart defects, and they vary greatly in severity and treatment approaches. Some of the most common CHDs include:
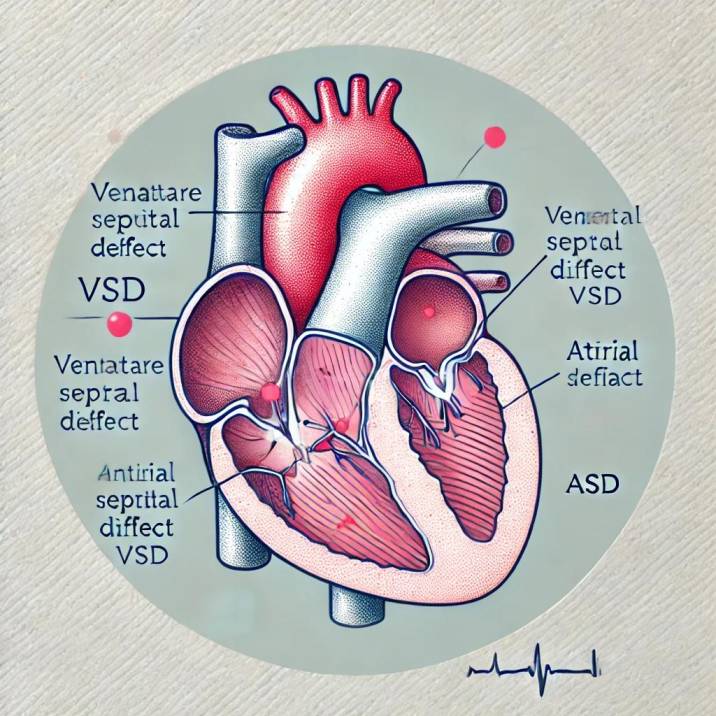
- Ventricular Septal Defect (VSD): A hole in the wall between the heart’s two lower chambers, causing abnormal blood flow.
- Atrial Septal Defect (ASD): A hole between the upper chambers of the heart, which can allow oxygen-rich and oxygen-poor blood to mix.
- Tetralogy of Fallot (TOF): A combination of four heart defects that result in poor oxygen flow to the body, often leading to cyanosis.
- Patent Ductus Arteriosus (PDA): A condition where the ductus arteriosus, a blood vessel that normally closes after birth, remains open and causes heart issues.
- Transposition of the Great Arteries (TGA): A serious condition where the two main arteries leaving the heart are switched, preventing oxygenated blood from reaching the body.
These are just a few examples, but they illustrate the diversity and complexity of congenital heart defects.
Treatment Options for Congenital Heart Defects
Treatment for CHDs depends on the type and severity of the defect. The goal is always to improve the baby’s heart function and ensure healthy blood flow. Here are the most common treatment approaches:
- Medication: In some cases, medications can help manage symptoms or stabilize the baby’s condition. For example, drugs may be used to lower blood pressure, remove excess fluid, or strengthen the heart’s pumping action.
- Surgical Intervention: Many CHDs require surgery, especially if the defect is severe. Open-heart surgery may be necessary to repair or close holes, correct valve problems, or reposition arteries. In some cases, catheter-based procedures can be used to make repairs without the need for open surgery, minimizing recovery time.
- Minimally Invasive Procedures: Thanks to advancements in technology, many CHDs can now be treated with less invasive procedures. For example, doctors may insert a catheter into a blood vessel to place a small device that repairs the defect.
New developments in pediatric cardiology mean that even the most complex heart defects can often be corrected, giving these babies a better quality of life.
Long-Term Care and Follow-Up for Babies with CHDs
Even after treatment, babies with CHDs need lifelong care. Regular follow-ups with a pediatric cardiologist are essential to monitor their heart health, ensure proper growth and development, and detect any potential complications.
- Routine Checkups: Regular cardiac evaluations, including echocardiograms and EKGs, are critical in monitoring heart function as the child grows.
- Developmental Monitoring: Some children with CHDs may experience developmental delays or issues with physical growth, which need to be addressed early on.
- Emotional Support: The journey with a CHD doesn’t just affect the child—it impacts the entire family. Many families find emotional support groups or counseling helpful as they navigate the challenges of living with a congenital heart condition.
Advances in Technology and Research in 2024 for CHD Treatment
The future of CHD treatment looks promising. With advancements in 3D printing, doctors can now create detailed models of a baby’s heart to plan surgeries more effectively. Stem cell research is also showing potential in regenerating damaged heart tissue, and robot-assisted surgeries are allowing for even more precise interventions.
In 2024, we’re seeing exciting developments in non-invasive procedures and gene therapies, opening up new possibilities for treating congenital heart defects that were once deemed too complex.
Conclusion:
Congenital heart defects may be daunting, but with early detection and advanced treatments, many newborns go on to live healthy and happy lives. From simple medications to complex surgeries, today’s healthcare system offers numerous ways to manage and correct these defects. If your baby has been diagnosed with a CHD, remember that you’re not alone—expert care and support are available every step of the way. Stay proactive, keep informed, and work closely with your child’s healthcare team to ensure the best outcome.




8 thoughts on “Congenital Heart Defects in Newborns: Diagnosis and Treatment”