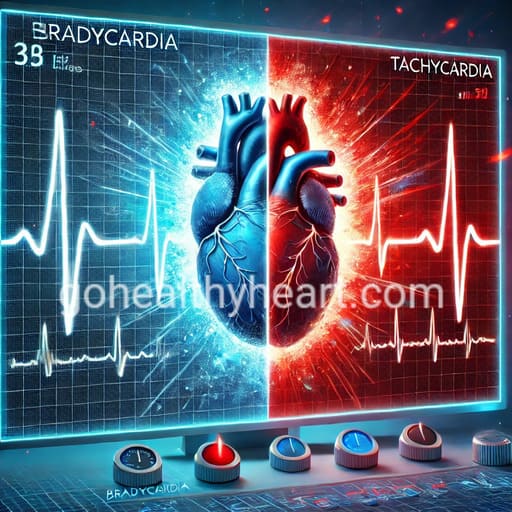
Bradycardia and Tachycardia: What’s More Dangerous?
By Dr. Nageswara Rao Goteti, Interventional Cardiologist
Introduction
The human heart is a remarkable organ that maintains life through its steady, rhythmic beating. This vital pump typically beats between 60 and 100 times per minute in adults, delivering oxygen-rich blood throughout the body. However, when this rhythm becomes disrupted, it can lead to conditions known as bradycardia and tachycardia – two distinct types of heart rhythm disorders that affect millions of people worldwide. Understanding bradycardia and tachycardia is crucial for recognizing early warning signs and seeking appropriate medical care.
Understanding Normal Heart Rhythm
Before delving into bradycardia and tachycardia, it’s essential to understand what constitutes a normal heart rhythm. The heart’s electrical system coordinates its contractions, with the sinoatrial node (SA node) acting as the natural pacemaker. This system typically maintains a steady rhythm that adjusts to the body’s needs, increasing during physical activity or stress and decreasing during rest.
A normal resting heart rate varies by age, fitness level, and overall health status. While most adults have a resting heart rate between 60 and 100 beats per minute, trained athletes might have lower rates due to their enhanced cardiovascular efficiency. Understanding these normal variations helps healthcare providers better diagnose and treat bradycardia and tachycardia when they occur.
The Impact of Heart Rhythm Disorders
Heart rhythm disorders, including bradycardia and tachycardia, can significantly impact a person’s quality of life. These conditions affect not only physical health but also emotional well-being and daily activities. When the heart beats too slowly (bradycardia) or too quickly (tachycardia), it can compromise the body’s blood supply, leading to various symptoms and potential complications.
Bradycardia: When the Heart Beats Too Slowly
Bradycardia occurs when the heart rate drops below 60 beats per minute. While this can be normal in some individuals, particularly well-conditioned athletes, it may indicate a serious condition in others. Understanding bradycardia and tachycardia patterns helps healthcare providers determine when slow heart rates require medical intervention.
The causes of bradycardia are diverse. Age-related changes often contribute through natural degeneration of the heart’s electrical system and fibrosis of cardiac tissue. Medical conditions such as coronary artery disease, heart attack damage, hypothyroidism, and inflammatory diseases affecting the heart can also cause bradycardia. Additionally, certain medications like beta-blockers, calcium channel blockers, and some sedatives may slow the heart rate.
Symptoms of bradycardia can range from mild to severe, depending on how slowly the heart beats and the underlying cause. Patients often experience persistent fatigue and weakness, dizziness, confusion, shortness of breath, chest pain, and in some cases, fainting episodes. Exercise intolerance and heart palpitations may also occur, particularly during physical activity.
Tachycardia: When the Heart Races
Tachycardia, the counterpart to bradycardia, occurs when the heart rate exceeds 100 beats per minute at rest. The relationship between bradycardia and tachycardia illustrates the complex nature of heart rhythm disorders, as some patients may experience both conditions at different times.
Several distinct forms of tachycardia exist, including supraventricular tachycardia (SVT), ventricular tachycardia, atrial fibrillation, and atrial flutter. Each type of tachycardia requires specific treatment approaches, making accurate diagnosis crucial for effective management.
Cardiovascular conditions such as heart failure, cardiomyopathy, high blood pressure, and coronary artery disease commonly cause tachycardia. Systemic conditions including hyperthyroidism, anemia, fever, and infection can also trigger rapid heart rates. Lifestyle factors play a significant role, with excessive caffeine consumption, alcohol use, smoking, and high stress levels all potentially contributing to tachycardia.
Comprehensive Diagnosis Approaches
The diagnosis of bradycardia and tachycardia requires a thorough medical evaluation. Healthcare providers employ various diagnostic tools to assess heart rhythm disorders accurately. The process begins with a detailed medical history and physical examination, during which doctors consider both bradycardia and tachycardia as potential causes of symptoms.
Modern diagnostic technology has revolutionized how medical professionals detect and monitor heart rhythm disorders. Standard tests include electrocardiograms (ECG), which provide immediate snapshots of heart activity, and Holter monitoring, which tracks rhythms over 24-48 hours. For intermittent symptoms, event monitors might be used over several weeks to capture episodes of bradycardia and tachycardia as they occur.
Advanced Treatment Options
Treatment approaches for bradycardia and tachycardia have evolved significantly in recent years. Medical professionals now have access to a wide range of interventions, from medication to advanced procedures. The choice of treatment depends on the specific type of rhythm disorder, its severity, and the patient’s overall health status.
Medication Management
Pharmaceutical interventions for heart rhythm disorders continue to advance. New medications with fewer side effects and more targeted actions help regulate heart rhythms more effectively. While traditional beta-blockers remain useful for tachycardia, newer variants offer more selective action with reduced impact on other body systems.
Technological Innovations
The field of cardiac rhythm management has seen remarkable technological advances. Modern pacemakers used for bradycardia are now smaller, more sophisticated, and can be monitored remotely. Similarly, implantable cardioverter-defibrillators (ICDs) provide life-saving therapy for certain types of tachycardia.
Prevention and Lifestyle Management
Managing bradycardia and tachycardia often requires a comprehensive approach that includes lifestyle modifications. Regular exercise, stress management, and proper sleep habits play crucial roles in maintaining healthy heart rhythms. Dietary considerations, including limiting caffeine and alcohol intake, can help prevent episodes of tachycardia.
Risk factor management is equally important in preventing complications from bradycardia and tachycardia. This includes controlling blood pressure, managing diabetes, maintaining a healthy weight, and avoiding tobacco use. Regular medical check-ups allow healthcare providers to monitor heart rhythm patterns and adjust treatments as needed.
Research and Future Developments
Ongoing research into bradycardia and tachycardia continues to yield new insights and treatment possibilities. Scientists are investigating genetic factors that may predispose individuals to heart rhythm disorders. Additionally, new technologies for monitoring and treating bradycardia and tachycardia are under development, promising more effective and less invasive options for future patients.
Frequently Asked Questions
Q: Can bradycardia and tachycardia occur in the same person?
A: Yes, some conditions like sick sinus syndrome can cause alternating periods of slow and fast heart rates. Understanding both bradycardia and tachycardia helps doctors provide comprehensive treatment in such cases.
Q: Are heart rhythm disorders life-threatening?
A: While not all arrhythmias are dangerous, some forms of bradycardia and tachycardia can lead to serious complications if left untreated. Regular medical evaluation is essential for proper management.
Q: Can lifestyle changes alone treat heart rhythm disorders?
A: Mild cases might improve with lifestyle modifications, but many patients require medical treatment. The management of bradycardia and tachycardia often requires a combination of approaches for optimal results.
Q: How do I know if my heart rate is abnormal?
A: While occasional variations are normal, consistently high or low heart rates, especially when accompanied by symptoms like dizziness or shortness of breath, warrant medical attention.
Q: Can children develop bradycardia or tachycardia?
A: Yes, heart rhythm disorders can affect people of all ages, including children. The causes and treatments may differ from those in adults.
When to Seek Emergency Care
Recognizing when to seek emergency care for bradycardia and tachycardia is crucial. Immediate medical attention is necessary if you experience severe chest pain, difficulty breathing, fainting or severe dizziness, sustained rapid heartbeat, or confusion. These symptoms could indicate a serious cardiac event requiring urgent intervention.
Conclusion
Understanding bradycardia and tachycardia helps patients recognize symptoms early and seek appropriate care. While some cases require immediate medical intervention, others can be managed through lifestyle modifications and regular monitoring. The key to successful management lies in proper diagnosis, appropriate treatment selection, and ongoing communication with healthcare providers.
As medical knowledge and technology continue to advance, the outlook for patients with bradycardia and tachycardia improves. Through careful management and regular medical supervision, most patients can maintain a good quality of life while effectively managing their heart rhythm disorders.
Remember that this information serves as a general guide, and individual cases may vary. Always consult with a qualified healthcare provider for personalized medical advice and treatment options.



