Blood Thinners After Heart Attack: Life-Saving Facts Revealed!
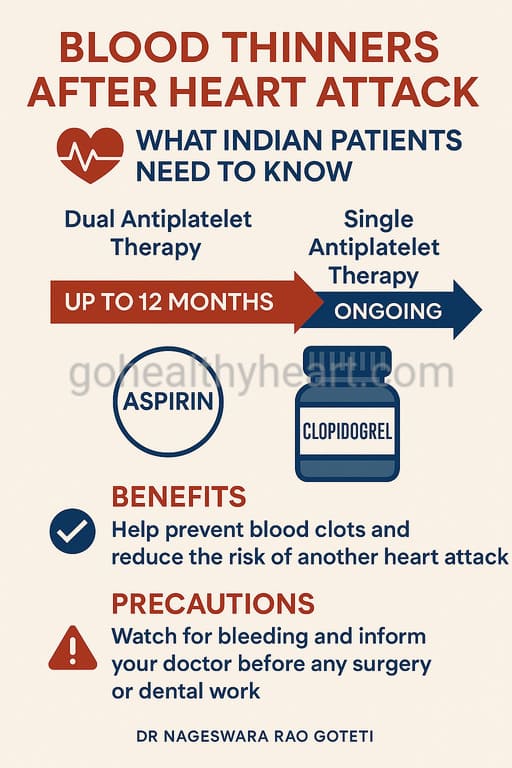
Table of Contents
- Introduction
- Understanding Blood Thinners After Heart Attack: The Basics
- Why Are Blood Thinners Essential After a Heart Attack?
- Types of Blood Thinners Commonly Prescribed in India
- Duration of Blood Thinner Therapy: How Long is Enough?
- Managing Side Effects and Bleeding Risks
- Lifestyle Guidelines for Indian Patients on Blood Thinners
- Special Situations: What Indian Patients Often Ask
- When to Seek Immediate Medical Help
- Balancing Benefits and Risks: The Personalized Approach
- Frequently Asked Questions About Blood Thinners After Heart Attack
- Conclusion: Empowering Indian Patients Through Knowledge
Introduction
When a heart attack strikes, it marks the beginning of a crucial recovery journey for patients and their families. The road to recovery often involves several medications, with blood thinners after heart attack being among the most critical. For many Indian patients, understanding these medications—their purpose, benefits, and management—can significantly impact long-term health outcomes.
As a cardiologist practicing in India, I’ve guided thousands of patients through their post-heart attack medication regimens. This comprehensive guide aims to provide Indian patients and their families with reliable, culturally relevant information about blood thinners after heart attack and their role in your cardiac care journey.
Understanding Blood Thinners After Heart Attack: The Basics
A heart attack (myocardial infarction) occurs when blood flow to a portion of your heart muscle becomes blocked, typically by a blood clot forming in an already narrowed coronary artery. This blockage deprives the heart muscle of oxygen, causing damage or death to heart tissue.
Blood thinners after heart attack work to prevent further clot formation. Despite their name, these medications don’t actually “thin” your blood but rather modify how your blood clots. For someone who has experienced a heart attack, these medications can be life-saving by significantly reducing the risk of recurrent cardiac events.
In the Indian context, where cardiovascular disease rates continue to rise and affect patients at younger ages compared to Western populations, proper adherence to blood thinners after heart attack can make a crucial difference in long-term survival and quality of life.
Why Are Blood Thinners Essential After a Heart Attack?
After experiencing a heart attack, your risk of developing new blood clots increases substantially. These clots can block arteries that are already narrowed by atherosclerotic plaque, potentially leading to another heart attack or even a stroke. Blood thinners after heart attack help prevent this dangerous scenario by interfering with your blood’s natural clotting mechanisms.
The importance of these medications becomes even more pronounced for patients who have undergone interventional procedures such as:
- Coronary angioplasty
- Stent placement
- Bypass surgery
For Indian patients specifically, several factors make blood thinners after heart attack particularly crucial:
- Higher rates of premature coronary artery disease
- Increased prevalence of metabolic syndrome and diabetes
- Unique genetic factors that may affect cardiovascular risk
- Challenges in accessing prompt emergency care in some regions, making secondary prevention critical
In my practice in Vijayawada, I’ve observed that patients who carefully follow their blood thinner after heart attack regimen typically experience significantly better outcomes than those who don’t.
Types of Blood Thinners Commonly Prescribed in India
Indian patients recovering from a heart attack may be prescribed one or more types of blood thinners. Understanding the difference between these medications helps in better compliance and management.
Antiplatelet Medications
These medications prevent platelets (tiny blood cells) from sticking together to form clots. Common antiplatelet medications prescribed in India include:
Aspirin (Ecosprin): Often the first-line antiplatelet agent prescribed after a heart attack. Available at affordable prices across India, making it accessible to most patients.
Clopidogrel (Clopitab, Plavix): Frequently prescribed alongside aspirin as part of dual antiplatelet therapy (DAPT), especially after stent placement.
Ticagrelor (Brilinta): A newer, more potent antiplatelet agent that may be prescribed for high-risk patients. Though more expensive than clopidogrel, generic versions are becoming increasingly available in India.
Prasugrel (Effient): Another potent antiplatelet that may be prescribed in specific cases, particularly for younger patients with diabetes who have undergone stenting.
Anticoagulants
These medications work by interfering with specific proteins in your blood that are involved in the clotting process. Common anticoagulants prescribed in India include:
Warfarin (Coumadin): An older anticoagulant that requires regular blood tests (INR) to monitor its effects. Still widely used due to its lower cost.
Novel Oral Anticoagulants (NOACs):
- Rivaroxaban (Xarelto)
- Apixaban (Eliquis)
- Dabigatran (Pradaxa)
These newer anticoagulants don’t require routine blood monitoring but are generally more expensive than warfarin. However, their availability as generic versions in India has increased accessibility for many patients.
Most Indian patients recovering from a heart attack will be on at least one antiplatelet medication (usually aspirin), with many requiring dual therapy for a specified period. The specific combination of blood thinners after heart attack will depend on your individual risk profile, the nature of your heart attack, interventions performed, and other health factors.
Duration of Blood Thinner Therapy: How Long is Enough?
One of the most common questions my patients ask is how long they need to continue taking blood thinners after heart attack. The answer varies based on several important factors:
- Type and severity of heart attack
- Whether a stent was placed and the type of stent
- Individual risk of bleeding
- Other underlying health conditions
- Overall cardiovascular risk profile
For most Indian patients, dual antiplatelet therapy (DAPT)—typically aspirin plus clopidogrel or ticagrelor—is continued for 6 to 12 months following a heart attack or stent placement. After this period, your cardiologist may recommend continuing with a single antiplatelet medication (usually aspirin) indefinitely.
However, it’s important to understand that these are general guidelines. The appropriate duration of blood thinners after heart attack therapy must be personalized for each patient. Factors that might influence a longer duration of therapy include:
- Multiple heart attacks
- Multiple stents or complex coronary intervention
- Ongoing high-risk features like diabetes or continued smoking
- Left main coronary artery or proximal LAD artery involvement
Conversely, patients with higher bleeding risks might require a shorter duration of dual therapy. The key message is to never stop or reduce your blood thinners after heart attack without explicit instructions from your cardiologist.
Managing Side Effects and Bleeding Risks
While blood thinners after heart attack provide crucial protection against future cardiac events, they do increase the risk of bleeding. Being aware of potential side effects and knowing how to manage them is essential for Indian patients.
Common Side Effects to Monitor
Blood thinners after heart attack may cause:
- Unexplained bruising or bruising more easily than usual
- Blood in urine (appearing pink, red, or brown)
- Blood in stool or black, tarry stools
- Nosebleeds that may last longer than normal
- Prolonged bleeding from cuts or injuries
- Heavy or prolonged menstrual bleeding in women
Special Considerations for Indian Patients
In the Indian context, several factors warrant special attention:
Gastrointestinal bleeding risk: This is a particular concern in India due to the widespread prevalence of H. pylori infection and the common use of non-prescription NSAIDs (pain relievers). If you have a history of ulcers, gastritis, or digestive issues, inform your doctor before starting blood thinners after heart attack.
Traditional remedies and supplements: Many Indian patients use Ayurvedic medicines, homeopathy, or other traditional remedies alongside prescribed medications. Some herbal products can interact with blood thinners, either increasing bleeding risk or reducing effectiveness. Always discuss all supplements with your cardiologist.
Cost considerations: For patients concerned about the cost of newer blood thinners, discuss this openly with your doctor. Generic alternatives or government assistance programs may be available to help manage expenses.
If you experience persistent or severe side effects while taking blood thinners after heart attack, contact your healthcare provider promptly. Never discontinue your medication without professional guidance.
Lifestyle Guidelines for Indian Patients on Blood Thinners
Living well while on blood thinners after heart attack involves more than just taking your medications as prescribed. Adopting heart-healthy habits enhances medication effectiveness and improves overall outcomes.
Dietary Considerations
Balanced Indian diet: Focus on heart-healthy options within the Indian cuisine:
- Whole grains like brown rice, whole wheat roti, and millets
- Plenty of vegetables and fruits
- Legumes and pulses for plant-based protein
- Limited use of coconut oil, ghee, and other saturated fats
- Reduced salt intake
Vitamin K consistency: If you’re taking warfarin, maintain consistent intake of vitamin K-rich foods (like green leafy vegetables). Sudden changes in consumption can affect your INR levels.
Alcohol moderation: Limit alcohol consumption as it can increase bleeding risk and interact with your medications.
Physical Activity Guidelines
Physical activity is crucial after a heart attack, even when taking blood thinners after heart attack. However, certain precautions are advisable:
- Begin with a supervised cardiac rehabilitation program if available
- Start with gentle walking and gradually increase intensity
- Avoid contact sports or activities with high fall risk
- Consider yoga (under proper guidance) as many asanas are safe and beneficial
- Stay hydrated, especially in India’s hot climate
Regular Monitoring and Follow-up
Regular check-ups are essential while on blood thinners after heart attack:
- If on warfarin, adhere to scheduled INR testing
- Keep all follow-up appointments with your cardiologist
- Maintain a record of any unusual symptoms or side effects
- Regularly check your blood pressure and heart rate
Medication Adherence Strategies
For many Indian patients, remembering to take multiple medications can be challenging. Try these approaches:
- Use pillboxes labeled with days of the week
- Set mobile phone reminders
- Link medication times to daily routines (e.g., after morning prayers or with meals)
- Ask a family member to help remind you
- Maintain a medication diary
Remember that blood thinners after heart attack work best when taken consistently and paired with heart-healthy lifestyle choices.
Special Situations: What Indian Patients Often Ask
Managing Blood Thinners Before Medical or Dental Procedures
Many patients worry about continuing blood thinners after heart attack when they need other medical procedures or dental work. The general guidance is:
- Always inform all healthcare providers about your blood thinner use
- For minor dental procedures, blood thinners can often be continued
- For major surgery, your cardiologist and surgeon will create a specific plan
- Never stop medications on your own before any procedure
Blood Thinners and Traditional Indian Remedies
The combination of allopathic blood thinners after heart attack with traditional remedies requires careful consideration:
- Some Ayurvedic herbs like turmeric, ginger, and garlic have natural blood-thinning properties
- When combined with pharmaceutical blood thinners, these may increase bleeding risk
- Always disclose all traditional remedies to your cardiologist
- A collaborative approach between modern medicine and traditional practices can often be achieved with proper medical supervision
Travel Considerations
Many Indians travel domestically or internationally for work, pilgrimages, or family visits. When traveling while on blood thinners after heart attack:
- Carry sufficient medication for your entire trip plus extra doses
- Keep medications in original packaging with prescriptions
- For international travel, research medical facilities at your destination
- Consider medical travel insurance
- If on warfarin, discuss INR testing options during extended travel with your doctor
When to Seek Immediate Medical Help
While taking blood thinners after heart attack, certain warning signs warrant immediate medical attention. Don’t delay seeking care if you experience:
- Severe or persistent headache
- Confusion or slurred speech
- Vomiting blood or material that looks like coffee grounds
- Black, tarry stools or bright red blood in stool
- Severe joint or muscle pain with swelling
- Unusual dizziness or weakness
- Any head injury, even if seemingly minor
In India, where access to emergency care can vary significantly between urban and rural areas, having an emergency plan is crucial. Identify the nearest hospital with emergency cardiac care capabilities and keep emergency contact numbers readily available.
Balancing Benefits and Risks: The Personalized Approach
The decision regarding which blood thinners after heart attack to prescribe and for how long requires balancing several factors:
- Prevention of future clots and cardiac events
- Individual bleeding risk
- Cost and accessibility of medications
- Comorbidities and other health conditions
- Patient preferences and lifestyle
While the benefits of blood thinners after heart attack outweigh the risks for most patients, the importance of personalized care cannot be overstated. This is why regular follow-up with your cardiologist is essential—it allows for medication adjustments based on your specific needs and response.
In my practice in India, I’ve observed that patients who understand their medications and actively participate in their care decisions show better compliance and outcomes. Don’t hesitate to ask questions about your blood thinners after heart attack or share concerns about side effects or costs.
Frequently Asked Questions About Blood Thinners After Heart Attack
Aspirin (often branded as Ecosprin) is the most commonly prescribed blood thinner, typically combined with clopidogrel (Clopitab) or ticagrelor (Brilinta) for the first 6-12 months after a heart attack. These medications prevent platelets from forming clots and are critical for preventing subsequent cardiac events.
Be cautious with pain relievers. Avoid NSAIDs like ibuprofen (Brufen) and diclofenac (Voveran) as they increase bleeding risk and may interfere with the cardioprotective effects of aspirin. Paracetamol (Crocin, Dolo) is generally considered safer, but always consult your doctor before taking any additional medications.
Yes, blood thinners can be safely prescribed for older patients, but with careful consideration of bleeding risk factors and potentially adjusted dosing. The benefits of preventing another heart attack often outweigh the risks, even in older individuals. Regular monitoring is particularly important for older patients on blood thinners.
If you remember within the same day, take the missed dose as soon as possible. If it’s almost time for your next dose, skip the missed one and continue with your regular schedule. Never take a double dose to make up for a missed one. If you frequently miss doses, discuss this with your doctor, as adherence to blood thinners after heart attack is crucial for preventing complications.
Yes, but your medications will need careful management. Inform your surgeon about all your blood thinners. For minor procedures, you may continue your medications, but for major surgery, your cardiologist and surgeon will create a specific plan that might involve temporarily stopping or adjusting your blood thinners to balance bleeding and clotting risks.
Food restrictions depend on the specific blood thinner. For warfarin users, consistency in vitamin K intake (found in green leafy vegetables like spinach, methi, and coriander) is important. For most other blood thinners like aspirin, clopidogrel, or ticagrelor, there are no specific food restrictions, but moderation with alcohol is advised for all patients
Typically, dual antiplatelet therapy (two blood thinners together) is prescribed for 6-12 months after a heart attack or stent placement. After this period, most patients continue with a single antiplatelet medication (usually aspirin) indefinitely. However, the exact duration is personalized based on your specific risk factors, type of stent placed, and bleeding risk assessment.
Newer agents like ticagrelor have shown some benefits over older medications like clopidogrel in clinical trials, particularly for high-risk patients. However, they are also more expensive. The “best” blood thinner varies by individual—factors including cost, other health conditions, and risk profile all matter. In India, where cost considerations are important, your doctor will help determine the most appropriate and affordable option for your situation.
Yes, you can travel, but preparation is key. Carry sufficient medication, relevant medical records, and your cardiologist’s contact information. For international travel, research medical facilities at your destination. If you’re on warfarin, discuss with your doctor how to manage INR testing during extended travel. Always consider medical travel insurance that covers pre-existing cardiac conditions.
Many Ayurvedic preparations contain herbs with blood-thinning properties, which could potentially increase bleeding risk when combined with pharmaceutical blood thinners. Always consult your cardiologist before starting any Ayurvedic, homeopathic, or other traditional medications. When possible, seek integrated care where your cardiologist and Ayurvedic practitioner can coordinate your treatment plan safely.
Conclusion: Empowering Indian Patients Through Knowledge
Taking blood thinners after heart attack represents a crucial step in your recovery journey and long-term heart health. These medications significantly reduce your risk of experiencing another cardiac event when taken appropriately and consistently.
As a cardiologist practicing in India, I understand the unique challenges our patients face—from medication costs to balancing traditional practices with modern medicine. The key to successful management lies in open communication with your healthcare team, understanding your medications, and active participation in your care decisions.
Remember that your blood thinners after heart attack work best when combined with heart-healthy lifestyle changes, regular follow-up care, and proper management of other cardiac risk factors like hypertension, diabetes, and cholesterol.
I encourage all patients and their families to ask questions, report any unusual symptoms promptly, and never discontinue medications without medical guidance. Your heart deserves the best care, and knowledge is an essential part of that care.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider regarding any medical conditions and before making any changes to your treatment regimen.