Angioplasty and Stenting: Key Differences You Need to Know
Introduction
Heart disease remains a leading cause of death worldwide, and two commonly performed procedures to restore blood flow in blocked arteries are angioplasty and stenting. While both treatments help manage coronary artery disease (CAD), they differ in their approach and long-term effectiveness.
If you or a loved one has been advised to undergo one of these procedures, understanding the differences between angioplasty and stenting is crucial. This article provides an in-depth comparison to help you make an informed decision.
What Is Angioplasty?
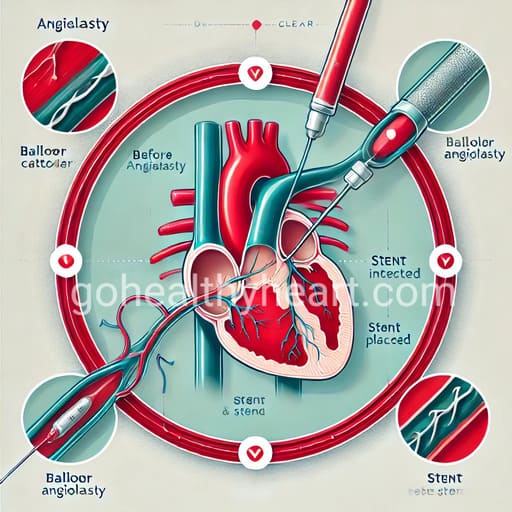
Angioplasty, also known as balloon angioplasty, is a minimally invasive procedure used to widen narrowed or blocked arteries. It involves inserting a thin tube (catheter) with a small balloon at its tip into the affected artery. Once in place, the balloon is inflated to push the plaque against the artery walls, improving blood flow. The balloon is then deflated and removed.
Learn more about how angioplasty is performed and its recovery process here.
When Is Angioplasty Recommended?
Angioplasty is commonly recommended in the following situations:
- To relieve symptoms of chest pain (angina) caused by reduced blood flow.
- To prevent a heart attack in patients with severe artery blockages.
- As an emergency procedure during a heart attack to quickly restore circulation.
Benefits of Angioplasty
- It is a minimally invasive procedure that requires only a small incision.
- The recovery time is shorter compared to open-heart surgery.
- It provides an immediate improvement in blood flow and reduces symptoms.
What Is Stenting?
Stenting is often performed alongside angioplasty to ensure the artery remains open. A stent is a small, mesh-like metal tube that is permanently implanted in the artery. After the balloon opens the blockage, the stent is expanded and left in place to prevent the artery from collapsing or narrowing again.
For a detailed explanation of the difference between angioplasty and stenting, refer to this resource.
When Is Stenting Recommended?
Stenting is typically recommended in the following cases:
- When the artery is at risk of re-narrowing after angioplasty.
- For multiple blockages or complex coronary artery disease.
- In cases where a previous angioplasty failed to keep the artery open.
Benefits of Stenting
- It prevents the artery from collapsing and reduces the risk of re-narrowing (restenosis).
- It provides long-term stability to treated arteries.
- It reduces the need for repeat procedures in high-risk patients.
Key Differences Between Angioplasty and Stenting
Although angioplasty and stenting are related procedures, they have some key differences.
- Angioplasty involves using a balloon to push plaque against the artery walls, whereas stenting involves placing a permanent metal mesh tube to keep the artery open.
- Angioplasty does not leave any permanent structure in the artery, while stenting provides long-term structural support. Because of this, arteries treated with angioplasty alone have a higher risk of re-narrowing, whereas stents help keep the artery open for a longer period.
- Angioplasty is often recommended for mild to moderate blockages, while stenting is preferred for severe or complex blockages where there is a higher risk of recurrence.
To understand the post-procedure recovery process for angioplasty and stenting, check out these medical guidelines.
Potential Risks and Complications
While both procedures are considered safe, they carry some risks.
Risks of Angioplasty
- There is a possibility of re-narrowing (restenosis) of the treated artery.
- The balloon inflation may cause blood vessel damage in some cases.
- Blood clots may form at the treated site.
Risks of Stenting
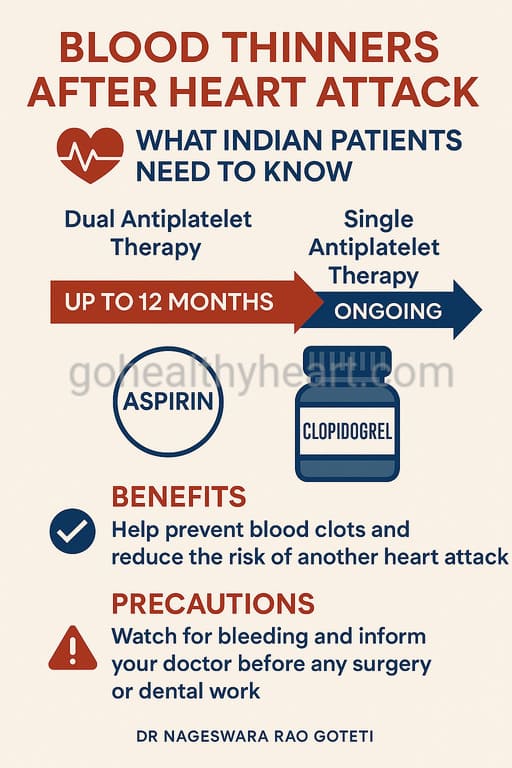
- There is a risk of blood clot formation around the stent, which may require blood-thinning medications.
- Some patients may experience an allergic reaction to the stent material (though this is rare).
- Scar tissue formation around the stent may lead to re-narrowing.
Recovery and Aftercare
Both procedures require lifestyle modifications and medications to maintain artery health.
After either angioplasty or stenting, patients are typically prescribed blood-thinning medications to prevent clot formation. Regular follow-up appointments are necessary to monitor the treated artery.
Patients are advised to adopt a heart-healthy lifestyle, which includes a balanced diet, regular exercise, and stress management. Avoiding smoking and managing underlying conditions like diabetes and high blood pressure are also crucial for long-term heart health.
For expert recommendations on angioplasty and stent placement recovery, refer to this trusted source.
Which Procedure Is Right for You?
The choice between angioplasty and stenting depends on several factors.
- If the artery blockage is mild, angioplasty alone may be sufficient.
- If there is a high risk of re-narrowing, stenting is usually the preferred option.
- Patients with multiple blockages or a history of recurring artery narrowing may benefit more from stenting due to its long-term effectiveness.
Ultimately, your cardiologist will assess your condition and recommend the most suitable procedure based on your specific heart health needs.
Final Thoughts
Both angioplasty and stenting are effective treatments for blocked arteries and can significantly improve heart health. While angioplasty alone may work in mild cases, stenting offers added stability and long-term benefits for many patients.
If you have been diagnosed with coronary artery disease, consult with an interventional cardiologist to determine the best course of action for your heart.
Authored by Dr. Nageswara Rao Goteti, Interventional Cardiologist, Vijayawada