Beta Blockers for Heart Disease: Safe or Risky?
Introduction
Heart disease continues to be one of the leading health challenges in India, affecting millions of families across our nation. As an interventional cardiologist practicing in Vijayawada for over two decades, I frequently encounter patients and their families seeking clarity about beta blockers for heart disease – one of the most commonly prescribed medications in cardiac care.
Beta blockers for heart disease represent a cornerstone of modern cardiovascular treatment, offering hope and healing to countless patients. These medications have transformed how we manage conditions like heart failure, high blood pressure, and recovery after heart attacks. Understanding how they work, their benefits, and what to expect can empower you to make informed decisions about your heart health journey.
This comprehensive guide will walk you through everything you need to know about beta blockers, from their mechanism of action to their specific role in managing various heart conditions prevalent in Indian patients.
What Are Beta Blockers and How Do They Work?
Beta blockers, medically known as beta-adrenergic blocking agents, are medications that work by blocking the effects of stress hormones like adrenaline on your heart and blood vessels. Think of them as protective shields that prevent your heart from being overstimulated by these hormones.
When you’re stressed, anxious, or physically active, your body releases adrenaline, which makes your heart beat faster and stronger. While this response is normal and necessary in certain situations, it can be harmful for people with heart disease. Beta blockers for heart disease step in to moderate this response, creating a calmer environment for your heart to function.
The mechanism is quite straightforward yet elegant. Beta blockers attach to specific receptors in your heart called beta-1 receptors, preventing adrenaline from binding to these sites. This results in several beneficial effects: your heart rate slows down, your blood pressure decreases, and your heart muscle doesn’t have to work as hard to pump blood throughout your body.
Key Benefits of Beta Blockers for Heart Disease
Improved Heart Function and Longevity
Research consistently shows that beta blockers for heart disease provide significant survival benefits, particularly for patients with heart failure and those recovering from heart attacks. These medications help prevent dangerous heart rhythms and reduce the risk of sudden cardiac death.
For patients with heart failure, beta blockers can actually help the heart muscle recover and become stronger over time through a process called reverse remodeling. This means that with consistent use, your heart’s pumping ability may improve, leading to better quality of life and reduced hospitalizations.
Enhanced Exercise Tolerance
Many patients worry that beta blockers will make them feel tired or limit their physical activity. While some initial fatigue is common, most patients find that their exercise tolerance actually improves over time as their heart becomes more efficient and symptoms like chest pain or shortness of breath decrease.
Blood Pressure Control
Beta blockers for heart disease are particularly effective in managing high blood pressure, especially in patients who also have elevated heart rates. This dual benefit makes them invaluable for Indian patients, who often present with both conditions simultaneously.
Types of Beta Blockers Commonly Used in India
Cardioselective Beta Blockers
These medications primarily target the heart without significantly affecting other organs like the lungs. Common examples include:
Metoprolol (Betaloc, Metolar): One of the most widely prescribed beta blockers in India, available in both immediate-release and extended-release formulations. It’s particularly effective for heart failure and post-heart attack care.
Bisoprolol (Concor, Bisomac): Known for its long duration of action, allowing once-daily dosing. It’s highly effective for heart failure and has excellent tolerability.
Nebivolol (Nebicard, Nebistar): A newer generation beta blocker that also has vasodilating properties, making it particularly suitable for patients with diabetes or those who experience sexual side effects with other beta blockers.
Non-Selective Beta Blockers
Carvedilol (Carca, Carvedon): This medication blocks both beta and alpha receptors, providing additional blood pressure-lowering effects. It’s particularly beneficial for patients with severe heart failure.
Propranolol (Inderal, Ciplar): While less commonly used for heart disease today, it remains valuable for certain arrhythmias and anxiety-related heart symptoms.
Specific Uses of Beta Blockers for Heart Disease
Heart Failure Management
Beta blockers for heart disease are essential in treating heart failure, particularly when the heart’s pumping function is reduced. They work by protecting the heart from harmful stress hormones that can worsen heart failure over time.
Starting beta blocker therapy in heart failure requires careful monitoring. We typically begin with very low doses and gradually increase them over several weeks to months. This approach allows your heart to adapt to the medication and minimizes side effects.
Post-Heart Attack Recovery
After a heart attack, your heart is vulnerable to further damage and dangerous rhythms. Beta blockers for heart disease provide crucial protection during this recovery period by reducing the heart’s workload and preventing electrical instability.
Recent studies have shown that the greatest benefit occurs in the first year after a heart attack, though many patients continue these medications long-term based on their overall cardiovascular risk profile.
Angina and Chest Pain
For patients experiencing chest pain due to coronary artery disease, beta blockers reduce the heart’s oxygen demand, leading to fewer episodes of angina and improved exercise capacity.
Arrhythmia Control
Beta blockers for heart disease are highly effective in managing various types of irregular heartbeats, from simple palpitations to more serious arrhythmias like atrial fibrillation.
Beta Blockers and Diabetes: Special Considerations for Indian Patients
Given India’s high prevalence of diabetes, it’s crucial to understand how beta blockers for heart disease interact with diabetes management. While older beta blockers could potentially worsen blood sugar control, newer agents like nebivolol and carvedilol are considered diabetes-friendly.
These medications can mask some symptoms of low blood sugar, particularly the rapid heartbeat that usually warns diabetic patients of hypoglycemia. Therefore, patients with diabetes need to monitor their blood sugar more closely and be aware of other warning signs like sweating, confusion, or shakiness.
However, the cardiovascular benefits of beta blockers for heart disease in diabetic patients typically outweigh these concerns, especially for those with established heart disease.
Managing Side Effects and Optimizing Treatment
Common Side Effects and Solutions
Most patients tolerate beta blockers well, but some may experience initial side effects that usually improve with time. Fatigue is the most common complaint, often lasting a few weeks as your body adjusts to the medication.
Cold hands and feet occur because beta blockers can reduce blood flow to extremities. This is usually mild and can be managed with warm clothing and gentle exercise.
Some patients experience vivid dreams or sleep disturbances, particularly with fat-soluble beta blockers like metoprolol. If this becomes problematic, switching to a water-soluble alternative like atenolol may help.
Monitoring and Follow-up
Regular monitoring is essential when taking beta blockers for heart disease. We typically check your heart rate, blood pressure, and overall symptoms every few weeks during the initial period, then every few months once you’re stable.
Blood tests to monitor kidney function and electrolytes are also important, especially if you’re taking other heart medications concurrently.
Lifestyle Modifications to Enhance Beta Blocker Effectiveness
Diet and Nutrition
A heart-healthy diet enhances the effectiveness of beta blockers for heart disease. Focus on fresh fruits, vegetables, whole grains, and lean proteins while limiting salt, saturated fats, and processed foods.
In the Indian context, this means enjoying traditional foods like dal, vegetables, and whole grains while being mindful of oil content and preparation methods.
Exercise and Physical Activity
Regular physical activity is crucial for heart health and can actually improve how well you tolerate beta blockers. Start with gentle activities like walking and gradually increase intensity as recommended by your doctor.
Since beta blockers lower your maximum heart rate, you may need to adjust your exercise targets. Instead of relying solely on heart rate, focus on how you feel during exercise – you should be able to have a conversation while being moderately active.
Stress Management
Chronic stress can worsen heart disease and counteract the benefits of medications. Incorporating stress-reduction techniques like meditation, yoga, or deep breathing exercises can complement your beta blockers for heart disease treatment.
When Beta Blockers May Not Be Appropriate
Contraindications and Cautions
While beta blockers for heart disease are generally safe and effective, they’re not suitable for everyone. Patients with severe asthma, certain types of heart block, or very low blood pressure may need alternative treatments.
If you have lung disease, your doctor will carefully weigh the benefits and risks, possibly choosing a cardioselective beta blocker and monitoring your breathing closely.
Drug Interactions
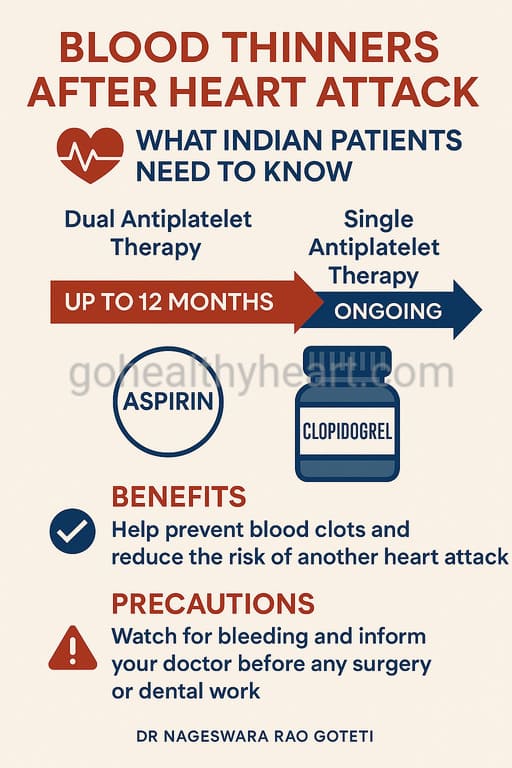
Beta blockers can interact with other medications, including some diabetes drugs, blood thinners, and certain antidepressants. Always inform your healthcare provider about all medications and supplements you’re taking.
The Role of Beta Blockers in Comprehensive Heart Care
Beta blockers for heart disease are rarely used alone. They’re typically part of a comprehensive treatment plan that may include ACE inhibitors, diuretics, and other heart medications. This multi-drug approach, often called guideline-directed medical therapy, provides optimal protection for your heart.
The key is finding the right combination and dosing for your specific condition and circumstances. This process requires patience and close collaboration with your healthcare team.
Recent Advances and Future Directions
The field of beta blockers for heart disease continues to evolve. Newer agents with additional properties, such as nebivolol’s nitric oxide-enhancing effects, offer improved tolerability and potentially better outcomes.
Research is ongoing into personalized medicine approaches, where genetic testing might help determine which beta blocker works best for individual patients.
Cost Considerations and Accessibility in India
Most beta blockers are available as generic medications in India, making them affordable for the majority of patients. Government schemes and insurance programs often cover these essential medications.
When cost is a concern, discuss this openly with your doctor. Often, equally effective generic alternatives are available at a fraction of the cost of brand-name medications.
Frequently Asked Questions About Beta Blockers for Heart Disease
1. How long do I need to take beta blockers after a heart attack?
The duration of beta blockers for heart disease treatment after a heart attack depends on several factors, including your heart function, other conditions, and overall cardiovascular risk. Recent studies suggest that the greatest benefit occurs in the first year, but many patients continue long-term therapy based on their individual risk profile. Your cardiologist will regularly assess whether continued treatment is necessary.
2. Can beta blockers cure heart disease?
Beta blockers for heart disease don’t cure heart disease but significantly improve outcomes by protecting your heart from harmful stress hormones. They can help prevent further heart attacks, reduce hospitalizations, and improve quality of life. In some cases, they may even help the heart muscle recover and become stronger over time.
3. Will beta blockers make me feel tired all the time?
Initial fatigue is common when starting beta blockers for heart disease, but this usually improves within a few weeks as your body adjusts. Many patients actually find their energy levels improve over time as their heart becomes more efficient and symptoms like chest pain or shortness of breath decrease.
4. Are beta blockers safe for elderly patients?
Yes, beta blockers for heart disease are generally safe for elderly patients, though they may require lower starting doses and more careful monitoring. The cardiovascular benefits often outweigh the risks, even in older adults. However, elderly patients may be more sensitive to side effects like dizziness or falls.
5. Can I take beta blockers if I have diabetes?
Modern beta blockers for heart disease, particularly vasodilating agents like nebivolol and carvedilol, are considered safe and effective for diabetic patients. While they can mask some symptoms of low blood sugar, the cardiovascular benefits typically outweigh this concern. Close blood sugar monitoring is essential.
6. What should I do if I miss a dose?
If you miss a dose of your beta blockers for heart disease, take it as soon as you remember, unless it’s almost time for your next dose. Never double up on doses. If you frequently forget doses, consider using a pill organizer or setting phone reminders.
7. Can beta blockers affect my exercise capacity?
While beta blockers for heart disease will lower your maximum heart rate during exercise, most patients find their overall exercise tolerance improves as their heart becomes more efficient. You may need to adjust your exercise targets and focus on how you feel rather than just heart rate measurements.
8. Are there natural alternatives to beta blockers?
While lifestyle modifications like regular exercise, stress management, and a heart-healthy diet are crucial for heart health, they cannot replace beta blockers for heart disease in patients who need them. However, these lifestyle changes can enhance the effectiveness of your medications and may allow for lower doses.
9. Can beta blockers cause weight gain?
Some patients may experience modest weight gain with beta blockers for heart disease, particularly with older agents. This is usually due to fluid retention rather than increased appetite. If significant weight gain occurs, contact your doctor as this could indicate worsening heart failure.
10. How do I know if my beta blocker is working effectively?
Signs that your beta blockers for heart disease are working include improved exercise tolerance, fewer episodes of chest pain, better blood pressure control, and overall improvement in how you feel. Your doctor will monitor objective measures like heart rate, blood pressure, and potentially heart function tests to assess effectiveness.
Conclusion
Beta blockers for heart disease represent one of the most important advances in cardiovascular medicine, offering proven benefits for millions of patients worldwide. For Indian patients dealing with heart disease, these medications provide hope for better outcomes and improved quality of life.
The key to successful treatment lies in understanding your medication, maintaining open communication with your healthcare team, and adhering to your prescribed regimen. Remember that beta blockers for heart disease are most effective when combined with healthy lifestyle choices and regular medical follow-up.
As we continue to advance our understanding of heart disease and its treatment, beta blockers for heart disease will undoubtedly remain a cornerstone of cardiac care. By working together with your healthcare team and staying informed about your treatment, you can maximize the benefits of these life-saving medications.
If you have questions about beta blockers for heart disease or any aspect of your cardiac care, don’t hesitate to reach out to your cardiologist. Your heart health is a journey, and we’re here to support you every step of the way.
For personalized advice about beta blockers for heart disease, consult with your cardiologist. This article is for educational purposes and should not replace professional medical advice.
About the Author: Dr. Nageswara Rao Goteti is an experienced Interventional Cardiologist practicing in Vijayawada, with extesnsive experience in managing complex cardiac conditions. He is committed to providing comprehensive, patient-centered care and educating families about heart health.