Heart Medication Duration: Expert Guidance for Effective Treatment

As an interventional cardiologist, I often encounter patients concerned about how long they need to continue their medications. Understanding the appropriate heart medication duration is crucial for effective treatment and long-term health outcomes. Many patients wonder if they can eventually stop their medications or if they’re destined for lifelong therapy. This comprehensive guide aims to provide clarity on medication timeframes while emphasizing that each treatment plan must be individualized based on specific factors related to your cardiac condition.
The Critical Importance of Following Prescribed Medication Timeframes
The duration for which heart medications are prescribed isn’t arbitrary. As a cardiologist, I determine treatment periods based on scientific evidence, clinical guidelines, and individual patient factors. Adhering to the recommended medication schedule is essential for preventing complications, managing symptoms effectively, and improving long-term prognosis.
When patients prematurely discontinue their cardiac medications, they risk serious consequences including symptom recurrence, disease progression, and even life-threatening events. Studies consistently show that adherence to prescribed treatment duration significantly reduces mortality and rehospitalization rates. For instance, patients who complete their full course of dual antiplatelet therapy after stent placement have substantially lower rates of stent thrombosis compared to those who stop early.
Personalized Approach to Cardiac Medication Plans
Each heart condition requires a tailored approach to treatment. What works for one patient may not be appropriate for another. When determining heart medication duration, I consider multiple factors:
The specific cardiac diagnosis plays a primary role in determining appropriate therapy duration. Acute conditions like myocardial infarction may require intensive but relatively shorter medication courses, while chronic conditions like heart failure often necessitate indefinite treatment.
Your overall health profile, including renal function, liver function, and comorbidities, significantly influences medication decisions. Patients with multiple comorbidities may require adjustments to standard treatment protocols.
Response to therapy also guides medication planning. If you show exceptional improvement, we might consider gradually reducing certain medications under close supervision. Conversely, suboptimal response might necessitate extending the treatment or adjusting the regimen.
Heart Medication Duration for Common Cardiac Medications
Understanding the typical timeframes for various cardiac medications can help patients set realistic expectations and improve adherence. Let’s explore the recommended durations for commonly prescribed medications.
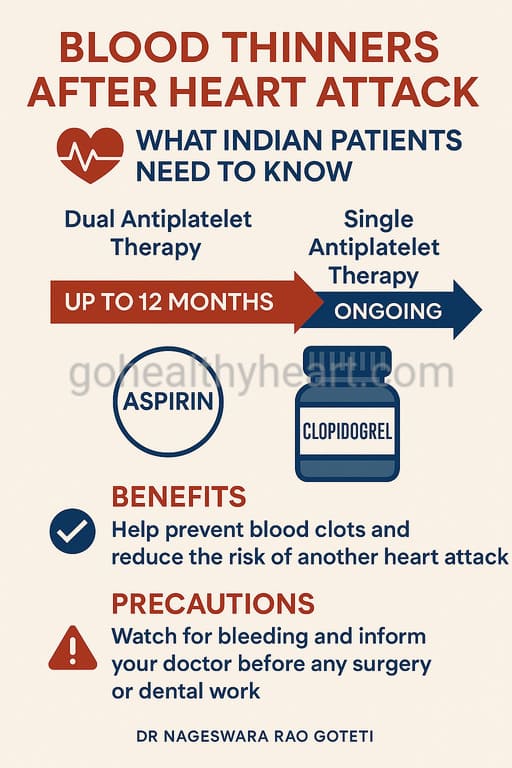
Antiplatelet Medications: Duration Guidelines
Antiplatelet medications like aspirin and clopidogrel represent a cornerstone of cardiovascular medicine. The treatment duration for these drugs varies significantly based on the underlying condition:
For primary prevention in high-risk individuals, low-dose aspirin may be prescribed long-term, though this approach is increasingly selective due to bleeding risks. The decision weighs cardiovascular benefits against potential complications.
Following acute coronary syndromes, dual antiplatelet therapy (DAPT) combining aspirin with a P2Y12 inhibitor typically ranges from 6-12 months. However, this period may be extended to 2-3 years in patients at high ischemic risk but low bleeding risk.
For patients who have undergone coronary stent placement, the DAPT duration depends on the stent type and the patient’s risk profile. Drug-eluting stents generally require longer treatment (12 months) compared to bare-metal stents (1-3 months).
In my practice, I’ve observed that careful monitoring during the prescribed period allows for timely adjustments based on individual response and tolerance.
Beta-Blockers: How Long Should You Take Them?
Beta-blockers are prescribed for various cardiac conditions, and their treatment duration varies accordingly:
Post-myocardial infarction, beta-blockers are typically recommended for at least 1-3 years, with many patients benefiting from indefinite treatment. The timeframe depends on factors like left ventricular function and overall recovery.
For heart failure with reduced ejection fraction, beta-blockers are usually lifelong medications. Their use is indefinite because they fundamentally alter disease progression and significantly improve survival.
When prescribed for hypertension, beta-blockers are typically long-term, though periodic reassessment may allow for modifications based on blood pressure control and the emergence of other risk factors.
I always emphasize to my patients that while the course for beta-blockers may be extended, regular follow-ups allow us to optimize the dose and evaluate continued necessity.
ACE Inhibitors and ARBs: Duration Considerations
ACE inhibitors and ARBs are beneficial for various cardiovascular conditions, and their treatment follows these general patterns:
For hypertension management, therapy is typically indefinite, though the specific agent or dose may change over time as other conditions develop or resolve.
Following myocardial infarction, particularly with left ventricular dysfunction, ACE inhibitors are recommended indefinitely. Lifelong treatment is advised because these medications significantly reduce mortality and prevent adverse cardiac remodeling.
In heart failure patients, these medications form part of the foundational therapy that improves symptoms, quality of life, and survival, warranting continuous use.
Diabetic patients with cardiovascular risk factors or nephropathy often receive ACE inhibitors or ARBs with an indefinite treatment plan to provide both cardiovascular and renal protection.
Statins: Long-term Considerations
Statins represent a critical class of medications for reducing cardiovascular risk, and their treatment follows these principles:
For secondary prevention in patients with established cardiovascular disease, statins are generally prescribed for life. The benefits of continued therapy outweigh the risks in most cases.
In primary prevention, the timeframe depends on risk assessment. High-risk individuals usually require indefinite therapy, while moderate-risk patients may warrant periodic reassessment based on evolving risk profiles.
Post-acute coronary syndrome, intensive statin therapy with indefinite continuation is recommended to stabilize plaque and prevent recurrent events.
Through my years of clinical practice, I’ve noted that patients who maintain their prescribed statin regimen experience fewer cardiovascular events compared to those who discontinue therapy prematurely.
Anticoagulants: Duration Based on Risk Assessment
Anticoagulants like warfarin, apixaban, and rivaroxaban have specific guidelines for treatment length:
For atrial fibrillation, therapy is typically lifelong, as the stroke risk remains as long as the arrhythmia persists. The decision balances stroke risk against bleeding risk using validated scoring systems.
Following venous thromboembolism, treatment ranges from 3-6 months for provoked events to indefinite for unprovoked or recurrent events. This strategy reflects the varying risk of recurrence based on the initial triggering factors.
Mechanical heart valves require lifelong anticoagulation with warfarin. The treatment cannot be shortened due to the persistent high risk of thromboembolism.
I carefully monitor patients on anticoagulants throughout their therapy, with regular assessments of both efficacy and safety parameters.
Unique Considerations Affecting Heart Medication Duration
Several special factors can modify the standard treatment recommendations:
Age-Related Treatment Adjustments
Older patients often require special consideration when determining medication plans:
The risk-benefit profile may shift with advancing age, potentially altering treatment decisions. For instance, bleeding risks with antiplatelets and anticoagulants increase with age, potentially shortening the optimal therapy duration.
Physiological changes affecting drug metabolism may necessitate dose adjustments rather than changes to treatment length.
Quality of life considerations become increasingly important in geriatric patients, sometimes influencing medication decisions.
Cardiac Medication During Pregnancy
Pregnancy with cardiac conditions requires careful treatment planning:
Some medications may need to be temporarily discontinued or replaced during pregnancy due to potential fetal risks, creating interruptions in the usual therapy.
Post-delivery, the treatment plan must be reassessed based on both maternal and child health considerations.
Medication adjustments during this period do not necessarily mean a permanent change to the intended course for the underlying condition.
Medication Considerations in End-Stage Disease
Patients with end-stage heart disease face unique treatment considerations:
Palliative approaches may modify medication goals to focus on symptom relief rather than long-term prevention.
Some preventive medications with delayed benefits may have their course shortened, while symptom-controlling medications usually continue.
The treatment plan becomes increasingly individualized based on goals of care discussions.
Strategies for Successful Adherence to Heart Medication Duration
Adhering to the prescribed treatment requires practical strategies:
Developing consistent routines around medication taking improves adherence to treatment plans. Simple techniques like using pill organizers or linking medication times to daily activities can significantly improve compliance with the intended regimen.
Understanding the purpose and importance of each medication in your treatment plan increases motivation to adhere to the regimen.
Regular follow-up appointments allow for assessment of adherence and provide opportunities to address concerns or side effects.
Family support systems play a crucial role in helping patients maintain their prescribed medication schedule, particularly for older patients or those with complex regimens.
When Medication Plans May Change
Several situations may warrant reconsideration of the initial treatment duration:
Development of Side Effects
If significant side effects occur, we may need to adjust the treatment plan:
Alternative medications within the same class might allow continuation of the intended therapy without the troublesome side effects.
Dose adjustments can sometimes mitigate side effects while preserving the benefits of the planned treatment.
In rare cases, severe side effects may necessitate premature discontinuation, shortening the therapy course.
Changes in Overall Health Status
As your health evolves, so might your medication requirements:
Development of new conditions might necessitate adjustments to your treatment plan to avoid drug interactions or address changing risk profiles.
Improvement in cardiac function might, in some cases, allow for reconsideration of certain medications.
Age-related changes in drug metabolism might require dose adjustments rather than changes to the intended treatment duration.
FAQs About Heart Medication Duration
Can I stop taking my heart medications once I feel better?
No, feeling better doesn’t necessarily mean you should discontinue your medications. Treatment duration is carefully determined based on the underlying condition, not just symptom control. Many cardiac medications work silently to prevent complications and progression of disease. Prematurely shortening your therapy can lead to symptom recurrence or serious complications. Always consult your cardiologist before making any changes to your medication regimen.
How does my doctor determine the appropriate duration for my cardiac medications?
Determining treatment length involves multiple factors including the specific diagnosis, severity of disease, risk factors, age, comorbidities, and response to therapy. I use evidence-based guidelines as a starting point for treatment decisions, then individualize based on your specific situation. Regular follow-ups allow me to reassess and adjust your medication plan as your condition evolves.
Are there any heart medications that I can safely stop taking after a certain period?
Some medications may have defined treatment periods. For example, dual antiplatelet therapy after stent placement typically has a recommended duration of 6-12 months, though this varies by individual risk factors. However, many cardiovascular medications, particularly those for chronic conditions like heart failure or atrial fibrillation, require indefinite use. Any consideration of discontinuation should be discussed with your cardiologist.
What should I do if I experience side effects from my cardiac medications?
If you experience side effects, don’t immediately discontinue your medication or shorten your treatment on your own. Instead, consult your cardiologist promptly. Often, adjustments to dosing, timing, or switching to alternative medications can resolve side effects while maintaining the intended therapeutic benefit. Your doctor can help determine whether the benefits of continuing the prescribed treatment outweigh the side effects.
How does aging affect my cardiac medication requirements?
As you age, your treatment plan may require adjustments due to changes in kidney function, liver metabolism, body composition, and increased risk of drug interactions with multiple medications. The therapy duration itself might not change, but dosages or specific medications might be modified. Regular follow-ups become increasingly important as you age to ensure your medication plan remains appropriate.
Can lifestyle changes reduce my need for long-term heart medications?
In some cases, significant lifestyle improvements like weight loss, regular exercise, smoking cessation, and dietary changes can impact medication needs. For conditions like hypertension or type 2 diabetes, substantial lifestyle modifications might allow for reduction in medication dosages or, occasionally, discontinuation of certain medications. However, this varies greatly by condition and individual factors. Any modifications to treatment should be physician-supervised.
How often should I have my cardiac medication plan reassessed?
The frequency of reassessment depends on your specific condition, stability, and the medications prescribed. Generally, newly diagnosed conditions or recent medication changes require more frequent evaluation, perhaps every 1-3 months. Stable, well-controlled conditions might need reassessment annually. Always follow your cardiologist’s recommended follow-up schedule.
Are generic heart medications as effective for the full treatment period?
Generic medications contain the same active ingredients as brand-name versions and are required to demonstrate bioequivalence. For most patients, generics provide equivalent effectiveness throughout the intended treatment duration. However, some patients may notice differences due to variations in inactive ingredients. If you switch between brand and generic during your therapy, monitor for any changes in effectiveness or side effects.
How does heart medication duration differ between children and adults?
Pediatric treatment considerations differ significantly from adults due to differences in metabolism, body composition, and the nature of pediatric heart conditions. Children with congenital heart defects may require different medication protocols than adults with acquired heart disease. Additionally, growth and development factors must be considered when planning cardiac treatment for pediatric patients.
Can I adjust my medication schedule during travel or special occasions?
Your treatment plan should remain consistent even during travel or special occasions. Plan ahead to ensure you have sufficient medication for the entire trip, plus extra in case of delays. If traveling across time zones, consult your physician about how to adjust medication timing while maintaining the integrity of your prescribed regimen. Never arbitrarily adjust your medication schedule for convenience.
Conclusion
Understanding and adhering to the appropriate heart medication duration is fundamental to successful cardiac care. As an interventional cardiologist, I’ve witnessed firsthand how proper adherence to treatment plans significantly improves outcomes and quality of life for my patients.
Remember that medication decisions represent a balance between providing maximum benefit while minimizing risks and side effects. Your treatment plan is individualized based on your specific condition, risk factors, and overall health status.
Open communication with your cardiologist about your medications is essential. Regular follow-ups allow for timely adjustments to your treatment plan as your condition evolves or as new evidence emerges.
By understanding the importance of proper medication duration and working closely with your healthcare team, you can optimize your cardiac health and improve your long-term prognosis. Your commitment to following the prescribed treatment is one of the most important factors in your cardiovascular health journey.